Produtos que agem no combate a bactérias são chamados de antibacterianos e geralmente divididos entre bactericida, bacteriostático e bacteriolítico.
Apesar da similaridade dentre os nomes, as definições estão diretamente relacionadas ao mecanismo de ação desses biocidas.
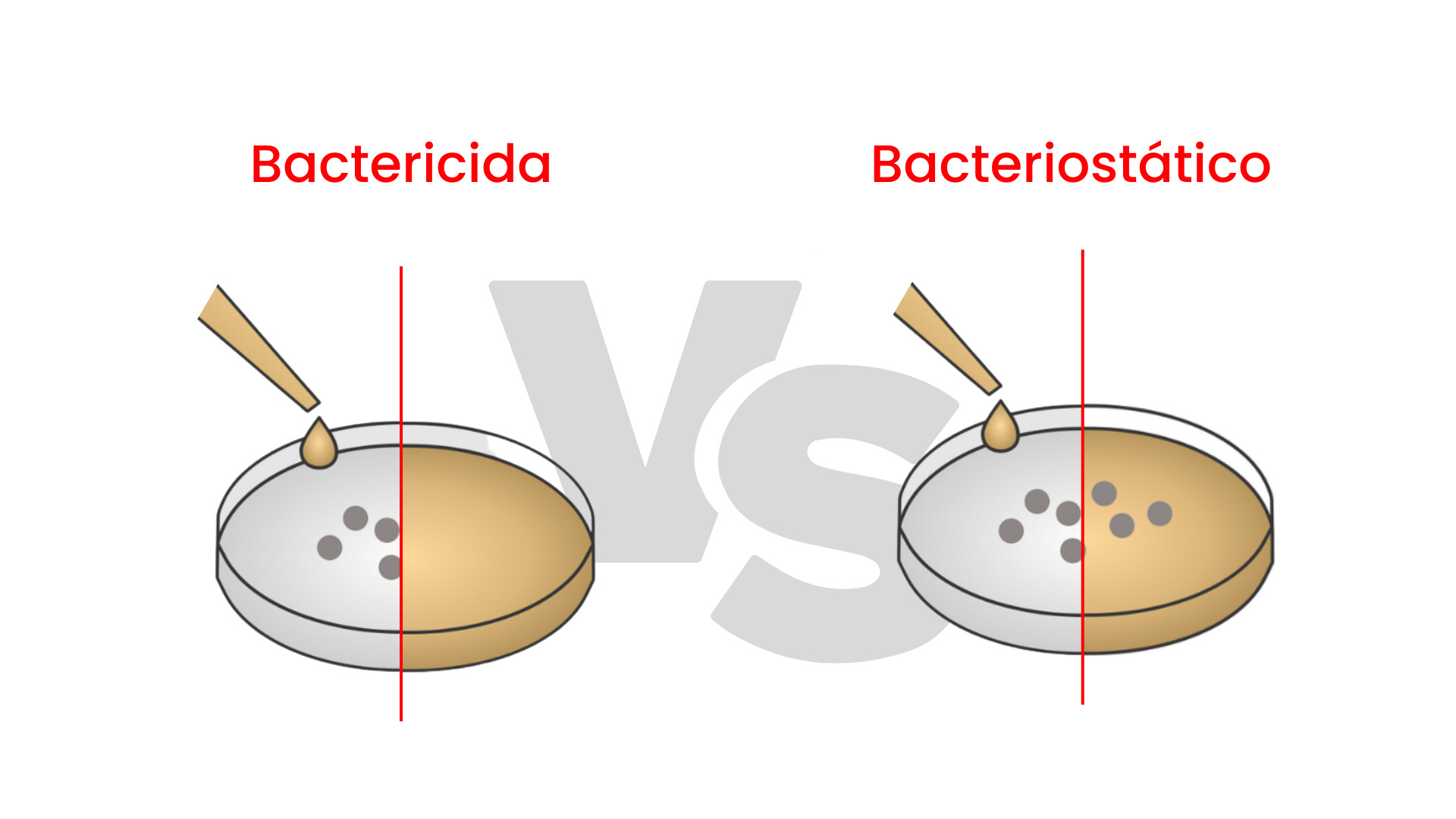
Um bactericida é um agente ou um composto que tem a capacidade de matar bactérias, sendo normalmente um produto químico, reduzindo significativamente sua proliferação.
Um produto é bactericida quando causa a morte de bactérias (em números até cerca de 99,99%) através de mecanismos específicos que atuam em seus processos vitais, como, por exemplo:
Já produtos como bacteriostáticos são aqueles que inibem o crescimento das bactérias no meio, sendo necessária atuação externa para eliminação das mesmas (tarefa do sistema imunológico na presença de organismos infecciosos no corpo humano).
Os bacteriolíticos, por sua vez, além de matar as bactérias ativas através do impedimento da formação da parede celular, também eliminam as células já mortas através de um processo natural que se chama lise celular - ou rompimento da célula bacteriana.
A penicilina, por exemplo, é classificada como um antimicrobiano bacteriolítico. Os antimicrobianos podem ser produzidos de forma natural por bactérias ou fungos ou podem ser totalmente sintéticos.
Definir um agente como bacteriostático ou bactericida não é uma tarefa tão trivial. Como diz a máxima, o “veneno está na dose”.
Em concentrações altas o suficiente, agentes conhecidos como bacteriostáticos podem ser potentes o suficiente para matar grande parte das bactérias quando estão bem concentrados – sendo considerados, portanto, como bactericidas.
De forma similar, aplica-se produtos bactericidas em pequenas concentrações e agir inibindo o crescimento de bactérias, ao invés de aniquilá-las, caracterizando o comportamento de um bacteriostático.
Desta forma, é extremamente importante a escolha do antimicrobiano correto na dose certa, a fim de otimizar ao máximo o processo de eliminação de bactérias.
Os bactericidas são indicados sempre que há risco de proliferação de bactérias capazes de comprometer a qualidade, segurança ou durabilidade de materiais e superfícies.
Sua aplicação é ampla e estratégica em diversos setores industriais, atendendo tanto às exigências normativas quanto às necessidades de performance do produto final.
O estudo de agentes antibacterianos possui avanços principalmente na área médico-hospitalar.
É comum neste âmbito classificar produtos bactericidas, bacteriostáticos ou bacteriolíticos como antissépticos, antibióticos ou desinfetantes.
Antissépticos são produtos que podem ser utilizados em corpos humanos ou animais (pele, mucosa, etc.) e agem em tecidos vivos para evitar infecções, sépsis ou putrefação.
Antibióticos, por sua vez, utilizam-se antimicrobianos no tratamento e prevenção de infecções bacterianas de maneira seletiva.
Ambos antissépticos e antibióticos podem assumir funções bactericidas ou bacteriostáticas. Já desinfetantes são agentes químicos antimicrobianos presentes em objetos e superfícies a fim de destruir microrganismos vivendo nesses objetos.
A aplicação desses agentes desinfetantes em superfícies de hospitais e clínicas é de suma importância para evitar o transporte de bactérias e agentes infecciosos de uma fonte até os pacientes vulneráveis à esse tipo de contaminação.
Para entendimento maior da gravidade dessas contaminações cruzadas, dados da OMS atestam que um milhão dos 234 milhões de pacientes operados por ano no mundo morrem em decorrência de infecção hospitalar.
Enquanto isso, a parcela de 7 milhões de pacientes apresentam quadros de complicação pós-operatória. (Pan American Healh Organization, 2010.)
No Brasil, os números assustam ainda mais.
Cerca de 14% dos pacientes contraem infecções hospitalares e 62% de pacientes internados em UTIs (Unidades de Terapia Intensiva) apresentam algum tipo de infecção - mais comum em unidades de parto.
Dentre os métodos presentes para eliminar bactérias em ambientes hospitalares cita-se o uso de produtos antimicrobianos comumente conhecidos como, por exemplo:
Álcool-gel para a assepsia das mãos (álcool etílico hidratado);
Água sanitária (hipoclorito de sódio);
Água oxigenada para desinfecção de pisos e aparelhos.
Já não tão populares, pode-se citar produtos contendo ativos com propriedades desinfetantes e bactericidas, por exemplo, o Triclosan (bactericida de amplo espectro de atuação), sais quaternários e biguanida.
Contudo, a ação desses ativos é imediata, sendo necessária o tratamento contínuo para assepsia e desinfecção a fim de garantir um ambiente hospitalar livre de contaminação cruzada.
Alternativamente, a linha de materiais com ativos antimicrobianos (comumente nanopartículas de prata) é uma tendência a ser mantida para, dessa forma, garantir atividade antimicrobiana na superfície desses materiais de forma permanente.
Veja - 7 aplicações da nanotecnologia
Materiais presentes em áreas de comum acesso em hospitais, por exemplo:
Podem receber o tratamento antimicrobiano por nanopartículas de prata e garantir eficácia permanente contra uma gama de bactérias patogênicas que causam infecções.
Confira - Pisos e laminados antimicrobianos: por que investir
Primeiramente, o efeito da nanoprata é eficiente mesmo em baixas dosagens - justamente pela característica geométrica em escala nano, a qual aumenta exponencialmente a área superficial ativa do aditivo.
O mecanismo de ação é semelhante ao de um composto bactericida: ataque a superfície da membrana celular da bactéria, penetrando no ambiente intracelular e impedindo tanto a respiração da bacteriana como a replicação do DNA.
Por fim, quando presente no interior da bactéria, gera-se os íons metálicos responsáveis pelo efeito microbicida final.
Somos referência mundial em nanotecnologia e inovação. Descubra como nossos aditivos podem elevar o padrão de suas operações e garantir resultados de alta performance aos seus produtos.
Entre em contato conosco e saiba mais sobre como a TNS Nano pode fazer a diferença para você!


Telefone:
+55 48 3236-5734
Interesse pela nossa tecnologia?
[email protected]
E-mail para contato:
[email protected]

